
There have been over 3200 cases of Monkeypox (mpox) in the UK since our first case back in May. The majority of these have been amongst gay, bi and other men who have sex with men, and most cases have been reported in London.
The great thing is that the cases were identified early on by the community, and we now know how to prevent and treat it. This hopefully means that we can get back to enjoying one another’s company sooner.
We’ve been supporting people to learn more about mpox and to get access to the vaccine, through info and advice sessions in bars, clubs, sex-on-premises venues, and hook-up apps across East London.
Take notice
Most cases are assumed to have been passed on through close skin-to-skin contact, including during sex. So this may mean getting up close in a bar or club too.

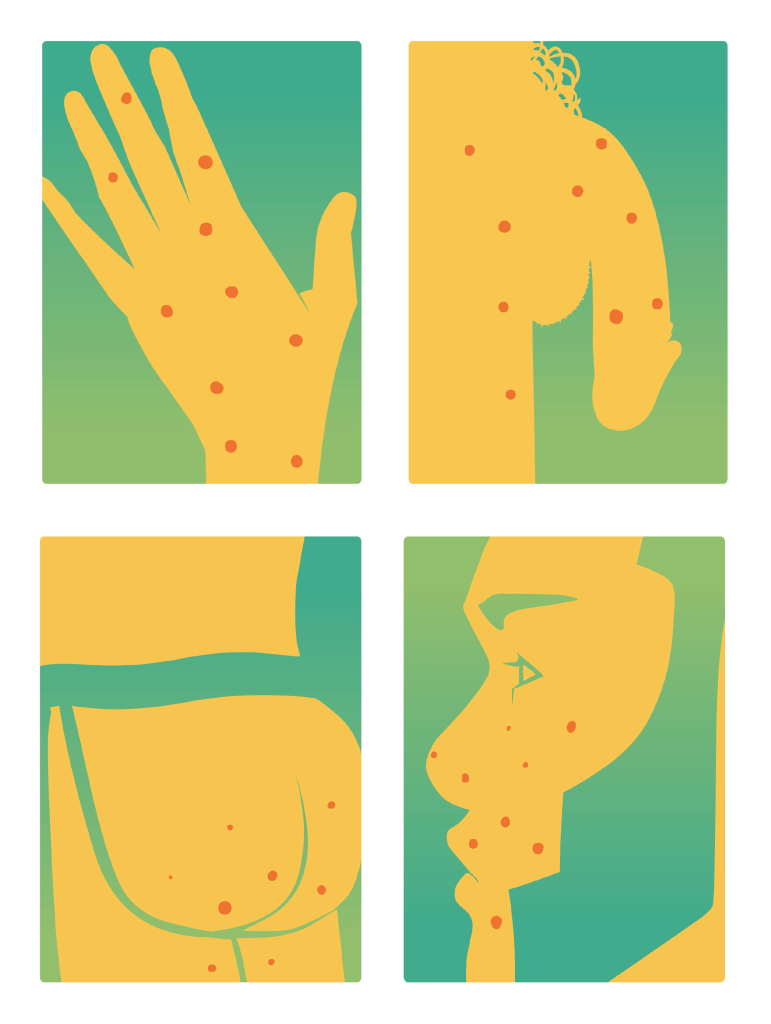
Not everyone experiences mpox in the same way or at the same time. Here’s some of the most common symptoms which usually present between 5-21 days after exposure:
- a rash around the mouth, penis, vagina, or bum, which may include blisters
- a high temperature
- a headache
- muscle aches
- backache
- swollen glands
- shivering (chills)
- exhaustion
- joint pain
- You may also have anal pain or bleeding from your bum
If you’re experiencing any of the above symptoms, particularly a rash, we’d advise staying at home and avoiding skin-to-skin contact or sharing bedding or towels with others. Call a sexual health clinic if:
- You have a rash with blisters, anal pain or bleeding from your bottom and have either:
- been in close contact, including sexual contact, with someone who has or might have MPox (even if they’ve not been tested yet) in the past 3 weeks
- had 1 or more new sexual partners in the past 3 weeks
- been to west or central Africa in the past 3 weeks
It can be frustrating not being able to hook-up particularly when you’re feeling horny, but there’s ways you can still get your fix whilst helping reduce the likelihood of mpox spreading:
- Scope out your body by yourself
- Whip out the sex toys
- Talk dirty over the phone or apps
- Take some pictures or get on a video call

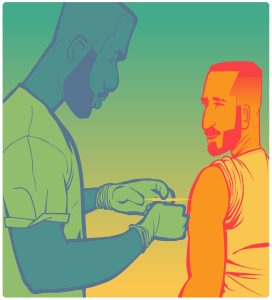
Vaccinate to prevent or treat
The best way to prevent the onward spread of mpox is to vaccinate. The vaccine is available for free through sexual health (GUM) clinics, and consists of 2 doses.
Vaccination has played a crucial role in protecting people and reducing case numbers. People who are eligible but have not yet received two doses of the vaccine are being encouraged to come forward and book their first dose by 16 June 2023 and be booked in for their second dose by the end of July 2023.
You learn more about the vaccine by contacting your local clinic by following this link: Find your nearest mpox vaccine
In East London clinics include:
- Ambrose King Centre (Tower Hamlets)
- Clifden Centre (Hackney)
- Sir Ludwig Guttmann Centre (Newham)
You can access the vaccine regardless of your immigration status.
The same vaccine is used to both treat and prevent mpox and is the same as used for smallpox, so you may see it referred to as the smallpox vaccine.
The vaccine can now be offered intradermal, which means it goes in closer to the skin’s surface which means it can get to the lymph nodes easier. It also requires less vaccine (fractional dosing means that they have up to 5 doses out of 1 vial) but is just as effective.
You may experience a small bump where the vaccine was administered. This is known as a bleb and usually goes down shortly after. If you’re nervous about this being seen by other people, you can ask for the vaccine to be administered higher up on your arm.
People living with HIV who are detectable and have a CD4 count of less than 200 will be offered the a full dose of the vaccine, not through intradermal. Please let the vaccinator know if this applies to you.
If you’ve had a 1 dose already, expect to be called back by that clinic at least 28 days after your 1st dose.
There may be a delay due to a focus on vaccinating more people with a 1st dose.

One of the best ways to break the chain of a virus being passed on, is to talk openly about it. There’s no shame if you have contracted mpox or any other virus for that matter. It’s always better to know because you can address it. It’s not the easiest thing to do, but by having a conversation with your sexual partners and friends you’re helping remove the fear with facts. Here’s a couple of ways we’ve done it:
- Tell them when you’ve had the vaccine and what your experience was like: ‘It was quick with few side effects and should be convenient to book too’
- Tell them if you’ve got symptoms: ‘Hey, I just wanted you to know I have been feeling great so I called a clinic and they think I’ve got mpox. I wanted you to know as I don’t want you to get ill and they advised anyone I was in close contact with, contacts the clinic for potential vaccine treatment’ They should then contact their sexual health clinic for the vaccine as PEP (post-exposure prophylaxis)
- Ask them if they’ve had the vaccine: ‘Hey, I had a great time with you last night and looking forward to next time. I forgot to ask whether you’d managed to the mpox vaccine? I’ve just booked mine in and thought I’d give you a heads up that there’s appointments at some clinics’
Stay informed
Monkeypox like any virus can change over time. It can present in different ways for different people which is why we’re keeping an eye on more info from UKHSA (UK Health Security Agency). We’ll be updating our page and social media as updates develop.
Here’s some of the other places you can keep an eye on for mpox info:
- UKHSA official Monkeypox guidance (including info on epidemiology, transmission, diagnosis, treatment and infection prevention and control): https://www.gov.uk/guidance/monkeypox
- Monkeypox resource page – Queer Health/The Love Tank: https://www.queerhealth.info/projects/monkeypox

If you’d like to support us to tell more people mpox, HIV and STIs in a sex-positive and non-judgemental way, why not volunteer with? Visit www.positiveeast.org.uk/volunteer to find out about our volunteer opportunities and to download an application form.